Beyond the Stereotypes - Understanding Addiction in 2025
Picture this: Sarah, a respected teacher and mother of two, began taking prescription pain medication after a car accident. Six months later, she was crushing pills to get through her daily routine. Her family couldn't understand how their loving, responsible Sarah had "chosen" this path. The truth? She hadn't chosen anything—her brain had been fundamentally altered by a medical condition called addiction.
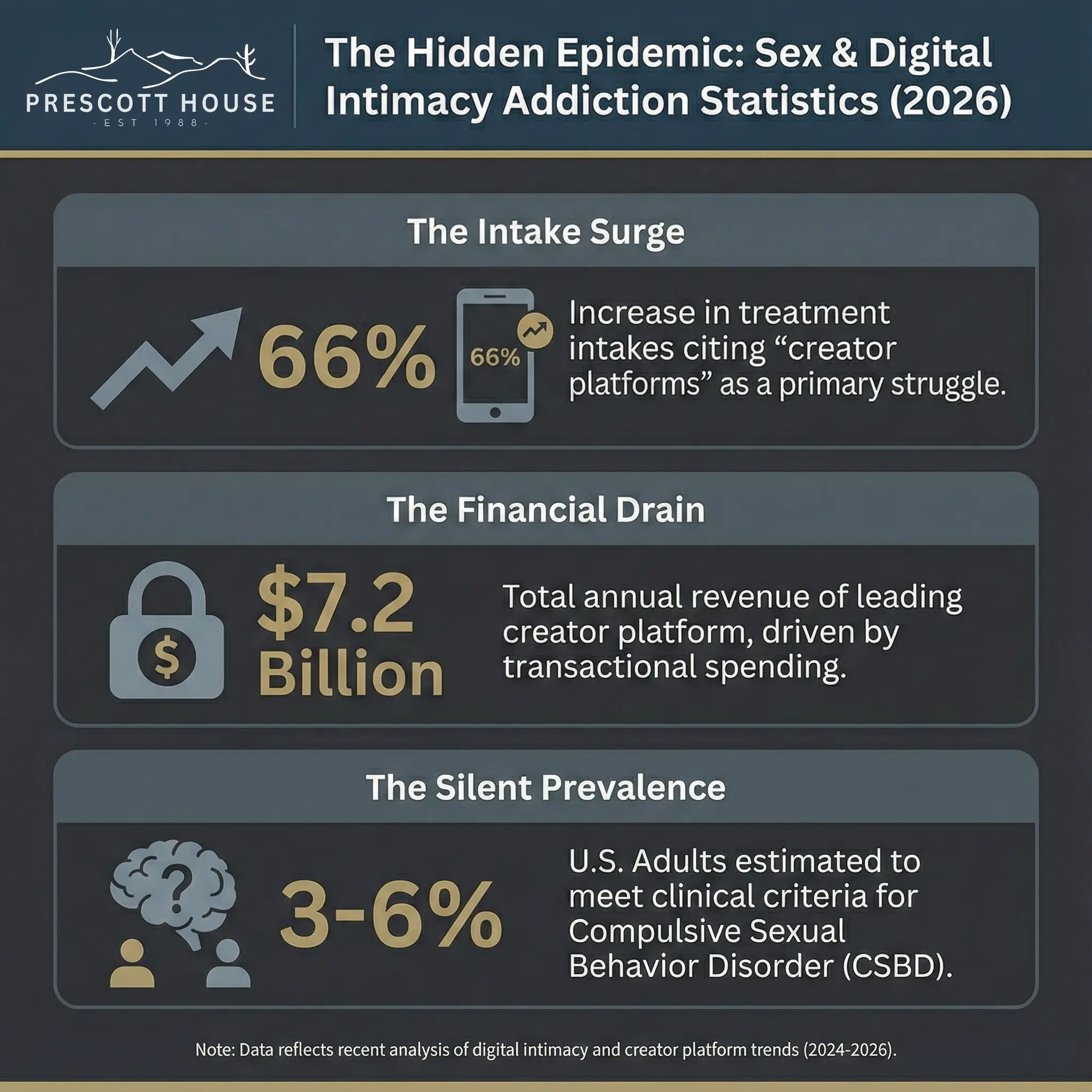
Sarah's story reflects a staggering reality. In 2023, an estimated 48.7 million people in the United States had a substance use disorder. Yet the majority never sought treatment, not because help wasn't available, but because shame and misunderstanding kept them trapped in silence. This isn't some distant social issue affecting "other people"—it's happening in our schools, our offices, our neighborhoods, and our families.
The misconceptions surrounding addiction create more than awkward conversations at dinner tables. They build walls of stigma that literally cost lives. When we perpetuate myths about addiction being a character flaw or a simple matter of willpower, we push people deeper into isolation precisely when they need support most. These harmful beliefs prevent millions from accessing the medical care they desperately need.

This post will systematically dismantle the most persistent and dangerous myths about addiction. We'll replace fiction with scientific facts, outdated stereotypes with current understanding, and judgment with compassion. Our goal isn't just to educate—it's to save lives by creating a world where seeking help for addiction feels as natural as seeking help for diabetes or heart disease.
What makes this discussion particularly relevant in 2025 is our rapidly evolving understanding of the brain, updated statistics that reveal the true scope of the crisis, and growing recognition that the language we use literally shapes treatment outcomes. We now know that words can either build bridges to recovery or create barriers that prove insurmountable.
Myth #1: Addiction is a Choice or a Moral Failing
Perhaps no myth causes more damage than the belief that people with addiction simply lack willpower or moral character. This perspective suggests that if someone "really wanted to quit," they could just stop. It's a seductive idea because it feels simple and maintains our sense that we control our own destinies.
The reality tells a completely different story. The National Institute on Drug Abuse defines addiction as a chronic, relapsing brain disorder characterized by compulsive drug seeking and use despite harmful consequences. This isn't medical jargon designed to excuse behavior—it's a description of measurable, physical changes in brain structure and function.
When substances enter the brain, they hijack the reward system that evolved to help us survive. They flood the brain with dopamine levels far beyond what natural rewards like food or social connection can provide. Over time, the brain adapts by reducing its natural dopamine production and decreasing the number of dopamine receptors. This creates a neurochemical environment where the person needs the substance just to feel normal, while everything else that once brought joy becomes muted.
These changes particularly affect brain circuits related to reward, stress, and self-control. The person may desperately want to quit—and they often do—but their altered brain makes this extraordinarily difficult. Initial drug use might have been voluntary, but continued use becomes compulsive as the brain's control mechanisms become compromised.
At Prescott House, we've witnessed this transformation countless times. Clients arrive convinced they're morally deficient, carrying shame that often proves more challenging to treat than the addiction itself. The relief in their eyes when they understand they have a medical condition, not a character defect, often marks the beginning of real healing.
Myth #2: You Have to Hit "Rock Bottom" Before Getting Help
The "rock bottom" myth might be one of the most dangerous beliefs circulating about addiction recovery. This persistent narrative suggests that people must lose everything—their job, family, home, health—before they're "ready" for treatment. Well-meaning friends and family often embrace this myth, believing they shouldn't "enable" their loved one by offering support until the person has suffered enough.
This thinking is not only cruel—it's medically irresponsible. We would never tell someone with diabetes to wait until they're in a diabetic coma before seeking treatment. We wouldn't suggest that someone with heart disease should wait for a massive heart attack before addressing their condition. Yet we routinely apply this backwards logic to addiction, a condition that can prove fatal while we're waiting for that mythical "bottom."
The truth is that early intervention dramatically improves treatment outcomes. The longer addiction progresses untreated, the more extensive the brain changes become, the more severe the physical health consequences grow, and the more damaged relationships and life circumstances become. Each day of untreated addiction makes recovery more challenging.
Research from the Journal of the American Medical Association shows that people who enter treatment earlier in their addiction journey have significantly higher success rates. They retain more of their support systems, maintain better physical health, and preserve more of their life structure—all factors that contribute to sustainable recovery.
At Prescott House, we've seen remarkable recoveries from individuals who sought help while they still had their jobs, their families, and their health intact. These clients often express gratitude that someone encouraged them to get help before their life completely unraveled. One client recently shared, "I thought I wasn't 'bad enough' for treatment because I still had my apartment and my family was still speaking to me. Now I realize those things became my foundation for recovery instead of things I had to rebuild from scratch."
The concept of "rock bottom" also ignores the reality that some people's bottom is death. Not everyone gets a dramatic wake-up call that motivates them to seek help. Many people struggling with addiction maintain relatively high functioning lives while slowly deteriorating inside. Others face such severe consequences early in their addiction that waiting for a lower bottom isn't realistic.
Instead of waiting for rock bottom, we should recognize these early warning signs that indicate treatment could be beneficial: using substances more frequently or in larger amounts than intended, spending increasing amounts of time obtaining or using substances, neglecting responsibilities or relationships, continuing to use despite negative consequences, or feeling unable to stop despite wanting to quit.
Myth #3: Treatment Only Works if You're Totally Ready
The belief that someone must be completely ready and motivated for treatment to succeed creates another barrier that delays potentially life-saving intervention. This myth suggests that unless someone is 100% committed and internally motivated to get sober, treatment will be a waste of time and money.
Real-world treatment outcomes paint a different picture entirely. Many people enter treatment feeling ambivalent, scared, or even resistant. They might be there because of family pressure, legal consequences, or workplace ultimatums rather than burning internal desire for sobriety. According to research published in the American Journal of Addictions, the source of motivation for entering treatment has little correlation with long-term success.
What matters more than initial readiness is what happens during treatment. Effective treatment programs work with people wherever they are emotionally and help them develop internal motivation. This process, called motivational enhancement, recognizes that ambivalence about change is normal and works to help people explore their own reasons for wanting recovery.
The stages of change model, developed by psychologists Prochaska and DiClemente, illustrates that readiness for change exists on a spectrum. People might be in precontemplation (not yet aware of the problem), contemplation (aware but ambivalent), preparation (intending to take action), or action (actively working on change). Effective treatment meets people wherever they are in this process.
Consider Marcus, who entered our program at Prescott House primarily to avoid jail time. He spent his first week arguing with counselors about whether he even had a problem. Through gentle exploration of his values and goals, he began to see connections between his substance use and his inability to maintain relationships with his children. By the end of treatment, his external motivation had transformed into genuine internal commitment to recovery.
This myth also discounts the power of external accountability and support. Sometimes the structure and expectations of treatment help people make changes they couldn't make on their own. The therapeutic environment provides safety, removes access to substances, and offers intensive support during the vulnerable early stages of recovery.
Even people who enter treatment reluctantly often discover that removing substances from their system allows them to think more clearly and connect with their authentic motivations. The fog of addiction often obscures people's genuine desires for health, connection, and meaning. Treatment can help clear that fog.
Breaking the Chains of Misinformation
Remember Sarah from our opening story? The teacher who found herself dependent on prescription medication after an accident? Her journey illustrates why dismantling addiction myths matters so profoundly. When her family stopped seeing her addiction as a moral failing and started understanding it as a medical condition, everything changed. They became allies in her recovery instead of obstacles. They offered support instead of judgment. They helped her access treatment instead of waiting for her to lose everything first.
The three myths we've explored today—addiction as a choice, the necessity of hitting rock bottom, and the requirement of complete readiness for treatment—represent just the tip of the iceberg. But they're among the most dangerous because they directly prevent people from seeking help when they need it most. When we believe these myths, we don't just misunderstand addiction; we actively contribute to a system that prioritizes punishment over healing, shame over support, and isolation over connection.
The scientific evidence is clear: addiction is a complex brain disorder that requires medical intervention, early treatment produces better outcomes than delayed treatment, and motivation can be cultivated during the treatment process. These aren't opinions or philosophical positions—they're facts supported by decades of research and millions of recovery stories.
Yet knowledge alone isn't enough. We must transform this understanding into action. This means changing how we talk about addiction in our families, workplaces, and communities. It means supporting policies that treat addiction as a health issue rather than a criminal one. It means offering compassion instead of judgment when someone we care about struggles with substance use.
Most importantly, it means recognizing that seeking help for addiction is a sign of strength, not weakness. It takes tremendous courage to admit you need support, to walk into a treatment facility, to commit to the difficult work of recovery. Every person who takes that step deserves our respect and encouragement, regardless of what brought them to that moment.
At Prescott House, we see the power of evidence-based treatment combined with compassionate care every day. We witness people rediscover their authentic selves, rebuild relationships they thought were lost forever, and create lives they never imagined possible. These transformations happen not in spite of addiction, but through the process of recovery—a process that begins the moment someone decides they deserve better.
If you or someone you love is struggling with addiction, don't wait for rock bottom. Don't assume you're not ready for help. Don't let shame or stigma delay the care that could save your life. Recovery is possible, hope is real, and support is available. The myths that have held so many people captive for so long don't have to hold you.
Your story of recovery could be the one that inspires others to seek help, that breaks the cycle of addiction in your family, that proves to the world that healing is always possible. It starts with a single phone call, a single conversation, a single moment of choosing hope over fear. That moment can be today.
References
- Myth - Understanding Addiction
- Drugs, Brains, and Behavior: The Science of Addiction
- Debunking Myths About Addiction Recovery
- Understanding Drug Use and Addiction DrugFacts | National Institute on Drug Abuse - NIDA
- A better way to say that: Stigmatizing language affects how we treat addiction - NIH MedlinePlus Magazine
- The Impact of Language on Stigma in Addiction and Mental Health - The Blanchard Institute